Connect With Us
Blog

Lupus and the Feet
 Lupus, an autoimmune disease, can significantly affect the bones, joints, and muscles in the feet, leading to various complications. This condition causes the immune system to attack healthy tissues, resulting in inflammation and damage. In the feet, lupus commonly leads to arthritis, causing joint pain, swelling, and stiffness. Tendonitis, an inflammation of the tendons, is also frequent, causing pain and difficulty in movement. Additionally, tendon laxity, or the loosening of tendons, can occur, causing instability and increasing the risk of sprains. One severe complication of lupus is avascular necrosis, where reduced blood flow to the bones leads to bone tissue death. This condition can cause severe pain and lead to bone collapse if untreated. Managing lupus symptoms requires early intervention and proper care. If you have this disease and are experiencing foot-related issues, it is strongly suggested that you schedule an appointment with a podiatrist for personalized treatment and to address your specific problems.
Lupus, an autoimmune disease, can significantly affect the bones, joints, and muscles in the feet, leading to various complications. This condition causes the immune system to attack healthy tissues, resulting in inflammation and damage. In the feet, lupus commonly leads to arthritis, causing joint pain, swelling, and stiffness. Tendonitis, an inflammation of the tendons, is also frequent, causing pain and difficulty in movement. Additionally, tendon laxity, or the loosening of tendons, can occur, causing instability and increasing the risk of sprains. One severe complication of lupus is avascular necrosis, where reduced blood flow to the bones leads to bone tissue death. This condition can cause severe pain and lead to bone collapse if untreated. Managing lupus symptoms requires early intervention and proper care. If you have this disease and are experiencing foot-related issues, it is strongly suggested that you schedule an appointment with a podiatrist for personalized treatment and to address your specific problems.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Landon Bowerbank, DPM from Pioneer Foot and Ankle. our doctor will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
Treatment Options for Ingrown Toenails

Ingrown toenails are characterized by the downward curling of the toenail's side or corner into the adjacent skin. An ingrown toenail typically results in redness, swelling, tenderness, and in some cases becomes infected. While frequently seen in the big toe, any toenail can become ingrown. The major causes of ingrown toenails include wearing ill-fitting footwear, improper nail trimming techniques, and traumatic injury to the toe. Seeking professional evaluation by a podiatrist is essential for an accurate diagnosis and appropriate treatment. For mild cases, conservative measures such as warm water soaks and placement of a cotton ball beneath the affected nail corner may provide relief. However, persistent or worsening symptoms warrant prompt intervention to prevent complications, including bacterial infection. In such instances, treatment may involve antibiotic therapy or, in severe cases, surgical removal of the ingrown portion of the nail. Among the ways to prevent an ingrown toenail are trimming nails straight and wearing shoes that fit properly. If you have an ingrown toenail, especially if pain is persistent, it is suggested that you schedule an appointment with a podiatrist for a complete exam and treatment suggestions.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Landon Bowerbank, DPM of Pioneer Foot and Ankle. our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenail Care
An ingrown toenail is a toenail that grows sideways into the nail bed, causing pain and swelling. Ingrown toenails can worsen and cause drainage, turning into a serious infection.
Several factors affect whether a person is at risk from an ingrown toenail. The many causes include being overweight, diabetes, participating in sports, having a fungal infection of the toe, and cutting your nails too short. Ingrown toenails also have a genetic predisposition, causing some people to be more prone to receive the condition than others. Other causes include improperly fitting shoes and shoes that keep the feet damp.
Ingrown toenails can be preventable with certain measures. For starters, allowing your toe nails to grow slightly longer in length will help prevent them from becoming ingrown. If you have already developed an ingrown toenail, soak the affected toe in warm water. This will alleviate the pain and help prevent an infection from forming. Antibiotic soap or Epsom salts may be added to further help the relieving process and avoid infection. Placing cotton beneath the affected area is also suggested, as this may help the toenail grow upwards and not into the nail bed. Swelling and redness can be reduced by resting with your feet elevated.
A podiatrist should be seen if the pain becomes so serious that it prevents you from doing your everyday activities. If a red streak running up your leg appears or if you suspect your infection has spread, contact a podiatrist immediately. Fast treatments can be undertaken to lessen your pain and have you walking comfortably.
An ingrown toenail can be easily treated with a Band-Aid. Simply wrap the affected toe with a Band-Aid to prevent infection and keep the nail from growing out at a painful angle.
In more serious cases, your podiatrist may decide to make a small incision to remove a portion of your toenail. To prevent the nail from growing back, medication will be placed directly into the nail bed. This procedure would be performed under local anesthesia and is a faster method to alleviate discomfort from an ingrown toenail. Post-procedure directions will have you stay off the affected foot for a day. Afterwards, normal activities can be resumed.
Essential Foot Care Tips for Elderly Individuals

As you age, elderly foot care becomes increasingly important for maintaining mobility and overall well-being. Elderly individuals are particularly susceptible to foot problems due to factors such as decreased circulation, thinning skin, and loss of natural cushioning. To promote foot health, it is essential for seniors to prioritize regular foot inspections, checking for any signs of redness, swelling, cuts, or sores. Keeping feet clean and moisturized can help prevent dryness and cracking, which can lead to infections. Wearing properly fitting shoes with adequate support and cushioning is vital for preventing foot pain and deformities. Additionally, it is beneficial for seniors to engage in gentle foot exercises, such as toe curls and ankle rotations, to improve circulation and flexibility. If foot pain or other conditions have developed, it is strongly suggested that you contact podiatrist who can offer relief methods and provide additional tips on elderly foot care.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Landon Bowerbank, DPM from Pioneer Foot and Ankle. our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly and their Feet
While proper foot care is important for everybody, senior citizens have the tendency to be more susceptible to certain foot conditions. The elderly should therefore be well informed about any problems that may arise and about what they can do to properly avoid or treat them.
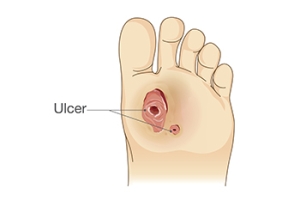
Some of the most common foot problems seniors are susceptible to include foot ulcers, ingrown toenails, fallen arches, and fungal nails. A foot ulcer is an open sore on the foot and can be a result of diabetes and decreased sensation in the feet. An ingrown toenail is defined as when the nail grows into the side of the toe. Fallen arches are indicated by the instep of the foot collapsing. A fungal nails is a condition that results in deformed and discolored toenails.
In order to avoid these conditions it is recommended that the feet be inspected by the patient on a regular basis. If these inspections are carried out routinely, there is a good likelihood that problems can be identified before they become severe, or can even be avoided altogether. If any abnormality is discovered, it is important that the individual consult a podiatrist for diagnosis and information on treatment options.
Proper foot hygiene is also important. Making sure that you always have clean, dry socks on can be a major deterrent to many different problems including bacterial infections, foot odor, and certain types of fungus. Wet feet are a major cause of many of these problems. If your socks get wet, it is important to change them. Walking around in wet socks may not only lead to various infections, but can irritate the skin and result in a number of various complications. Clean, dry feet are less likely to be affected by fungal and other infections.
As people age, the fat present on your feet begins to deteriorate. The protective nature of this fat keeps the feet healthy by providing a barrier between your bones and the ground. This also aids in giving the skin on the feet a certain amount of elasticity. This is one factor that causes elderly people to develop some serious foot issues. Foot moisturizers can be helpful to avoid certain problems associated with this. However, water-based moisturizers do not work as well for elderly people as they do for the young. Instead, it is more effective to use an emollient instead. An emollient is effective because it binds the water in the foot, keeping it from becoming absorbed too readily which will result in dry skin. Emollients also have a special property called occlusion, which provides a layer of oil on the skin. This layer prevents the foot from drying up and can be very effective in treating dry skin disorders. If you can keep the skin on your feet healthy, this will substantially reduce the number of foot problems you will encounter in old age.
Proper footwear is another way to keep feet healthy. Shoes that fit well and provide proper support help prevent ingrown toenails and fallen arches.
Certain medical conditions such as diabetes or poor blood circulation increase the risk for foot issues. For individuals with any of these conditions it is extremely important to conduct regular foot inspections to make sure that there are no sores or infections present.
Help for Non-Healing Diabetic Foot Ulcers
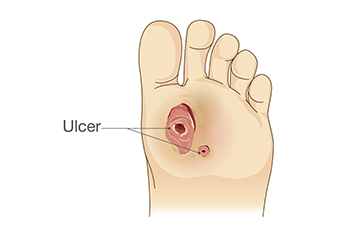
Non-healing foot ulcers in diabetic patients are influenced by a myriad of factors, including the wound environment, the patient's general health, and the medications they are taking. A compromised wound environment, often characterized by high bacterial load, excess moisture, or inadequate blood supply due to peripheral arterial disease, can impede healing. Additionally, the patient's overall health status plays a significant role, with conditions like obesity, smoking, and immune system deficiencies hindering the body's ability to repair tissues. Medications such as corticosteroids and certain chemotherapeutic agents may also interfere with wound healing processes. Addressing these multifaceted challenges requires a comprehensive approach, encompassing wound debridement, infection control, and optimizing the patient's general health through lifestyle modifications and medication adjustments. If you suffer from diabetic foot ulcers, it is strongly suggested that you are under a podiatrist to enhance healing outcomes and reduce the risk of serious complications.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Landon Bowerbank, DPM from Pioneer Foot and Ankle. our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Ease Painful Feet With Orthotics

Custom orthotics can be used to relieve foot pain and discomfort. They're also used to treat various foot conditions and deformities. Flat feet, bunions, and Morton's neuroma are just a few of the foot conditions that have been known to benefit from the use of orthotics.
Comfy feet are happy feet! Contact us today.
Athlete’s Foot Treatment
 Athlete's foot, a fungal infection of the skin on the feet, is usually treated with different types of antifungal medications. These can come in the form of creams, sprays, and powders, as well as oral medications for more severe cases. These treatments can kill the fungus that causes the infection. The infection usually clears up within a few weeks of topical treatment application. Keeping your feet clean and dry when treating athlete’s foot is important, as the fungus thrives in moist environments. Changing socks regularly, using antifungal powders in shoes, and avoiding walking barefoot in public areas, such as locker rooms or swimming pools, can help prevent the spread of the infection. A podiatrist, or foot doctor, might recommend a stronger prescription medication for more persistent cases. Podiatrists can also guide proper foot hygiene to prevent recurrence. If you are struggling with athlete’s foot, it is suggested that you consult a podiatrist for the right treatment options for you.
Athlete's foot, a fungal infection of the skin on the feet, is usually treated with different types of antifungal medications. These can come in the form of creams, sprays, and powders, as well as oral medications for more severe cases. These treatments can kill the fungus that causes the infection. The infection usually clears up within a few weeks of topical treatment application. Keeping your feet clean and dry when treating athlete’s foot is important, as the fungus thrives in moist environments. Changing socks regularly, using antifungal powders in shoes, and avoiding walking barefoot in public areas, such as locker rooms or swimming pools, can help prevent the spread of the infection. A podiatrist, or foot doctor, might recommend a stronger prescription medication for more persistent cases. Podiatrists can also guide proper foot hygiene to prevent recurrence. If you are struggling with athlete’s foot, it is suggested that you consult a podiatrist for the right treatment options for you.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Landon Bowerbank, DPM from Pioneer Foot and Ankle. our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.